I had an incredibly talented operative team available. Despite being staffed with two general surgeons, one orthopaedic surgeon, and an internist, we were able to troubleshoot difficulties and come up with solutions that would aim to provide care as close to our Western “standard of care” as possible in our austere environment. This was our solution: We ordered an inferior vena cava (IVF) filter from a higher level care facility in the region and our surgeons learned how to place a tulip IVF.





Now approximately one week post-injury, we performed an antegrade IMN of Khan’s left femur fracture through an enoxaparin window and chose a lateral position because of Khan’s body size. We didn’t have a fracture table, so we had to be creative. I felt particularly lucky because previous surgeons were nailing without the benefit of a C-arm (X-ray image intensifier), which is particularly challenging. They had to resort to a modified open technique.
In other patients, to nail supine with a standard Steris OR table, we reversed the table and placed the head extension on the foot. This allowed C-arm imaging proximally. We did not have a well leg holder, but found that a well-padded Mayo stand with the hip and knee of the well leg flexed actually worked – but barely. We would tape sand bags to the Mayo base to prevent the C-arm from knocking it over when coming in for lateral. (I recommend making sure you can image everything you need ahead of time before prepping, and of course, telling your C-arm operator exactly what you want him or her to show you.)
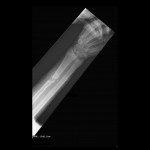
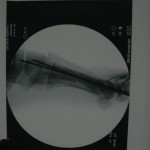
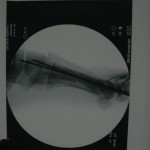
In this patient, our decision to nail in the lateral position made the procedure easier for this portly patient. We used blankets to pad the lower leg, which made a very stable platform on which to rest the operative leg. I made sure to leave space to feel the knee and ankle – this allowed me to assess length to some degree. Imaging through the table worked out well; just make sure the patient is moved down as far as possible to maximize C-arm access. The “bigger” femur is the operative side when viewed on the image intensifier. Make sure you have an axillary roll and care for the arms well.
If you have problems getting the shaft out to length, my plan was to use a sterile Kirschner bow and a couple of strong techs either scrubbed in or pulling rope off the field. If we had a femoral distractor, that could have been used. Another alternative would be the Stryker Hoffman external fixator to hold length/reduction while you get the guide wire across.







You can see that the AP and lateral imaging in this position is reasonable. The fixation in the proximal segment was just barely adequate, given the location of the proximal extent of the fracture. I decided to use an endcap extension on the proximal end of the Stryker T2 nail that allowed for theoretically optimal stabilization of the proximal segment with this technique.
Just over a week post-injury, we performed ORIF for Khan’s pilon fracture and pinned his segmental metatarsal fractures.



Khan was then transferred to a regional Afghan National Army hospital for rehabilitation and mobilization. He was stable and in good spirits about mobilization.
Post-nailing assessment suggested a 9 mm leg length discrepancy through the femur and his rotation appeared clinically symmetric. My assessment was that I likely ended shortening him a bit on the right side (retrograde). While not perfect, I do think we did the best we could for him in our facility.